Back at the start of term, the Badger brought to you the exciting news of a breakthrough in the research of CRISPR techniques from the Salk Institute California. This concerned the use of non-homologous end joining (NHEJ) to help medical researchers in their quest to cure genetic abnormalities, which had previously only been possible in non-dividing cells.
In short, the CRISPR system, developed from a bacterial immune defence system, uses nucleases to break apart faulty DNA, then copies a newly edited template DNA strand into the genome, to restore functionality. The NHEJ technique allows this without a template, and simply stick the two broken ends back together.
More broadly however, CRISPR can be used as a targeted DNA editing technique. Whereas previous methods involve retroviruses, which are not as specific and can potentially cause unwanted mutations, CRISPR foregoes this possible banana skin.
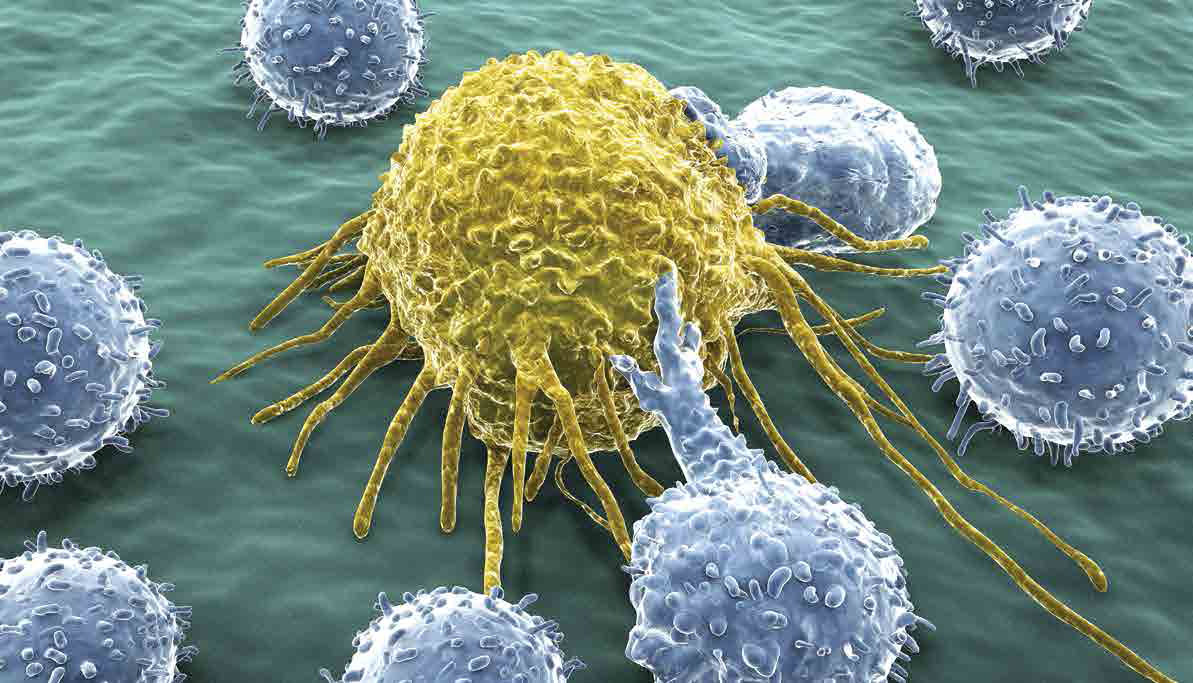
CRISPR also has tremendous potential in cancer treatments as well, as was recently shown by a paper in Nature, by Michel Sadelain, M.D., Ph.D., of Memorial Sloan Kettering Cancer Center, and his colleagues. They edited human T-cells, a form of white blood cell that kills potentially harmful cells, to express chimeric antigen receptor proteins (CARs). These proteins allow the T-cells to recognise and attack cancer cells that expressed a similar antigen, a type of protein marker.
The therapy in question takes a patient’s own T-cells, then modifies them to give them CARs, and returns them to their blood.
The CRISPR editing technique is essential to the success of the therapy, as it allows the lab workers to specifically place the CARs in the T-cell receptor alpha chain (TRAC) gene. When tested, the CRISPR/CAR cells outperformed both unmodified T-cells and T-cells that had the gene inserted by a retrovirus, a type of virus that can also be used to edit DNA. The precision of the CRISPR editing was the key, allowing much higher expression of the CAR proteins. Furthermore, the CRISPR/CAR cells were less likely to lose the recognition of the cancer cells, known as “exhaustion”, a phenomenon seen in many previous genetically altered T-cells.
James Kochenderfer M.D., P.H.D., who develops T-cell therapies for the NCI’s Centre for Cancer Research, also noted the importance of the precision for future works, “The finding that the location of CAR gene insertion can affect T-cell function is particularly intriguing. New gene-editing technologies will likely lead to rapid improvement in antigen-targeted T-cell immunotherapies for cancer.”
One of the greatest successes of the treatment was noted by Marcela V. Maus, M.D., Ph.D., of Harvard Medical School, which was the less risky approach that CRISPR editing facilitated. The ability to target specific locations may “prove safer than random integration, which carries the potential risk of generating a harmful mutation,”
Not only will this have potential implications for cancer research, other diseases may be able to be targeted by the CARs. The T-cells are the immune systems “enforcers”, they respond to all manner of bacterial and viral infections, so there may be an exponential number of antigen based locations that can enable taylor-made treatments to all manner of diseases.